Prof. Dr. Ignacio Rubio
Department of Anesthesiology and Intensive Care Medicine


Sepsis represents a lethal syndrome caused by a dysregulated und disproportionate immune reaction to infection. The intricacies of the sepsis–associated host immune response and the often concomitant multiple organ failure (MOF) underlie high mortality (sepsis is the major cause of death in ICUs!) and the extremely limited number of treatment options. In the acute phase of sepsis, the host response often manifests as a hyper-inflammatory burst (also known as “cytokine storm”) involving the profuse release of pro-inflammatory mediators. This can cause hemodynamic complications leading to endothelial barrier dysfunction all of which can further boost immune alterations, eventually culminating in organ failure and death.
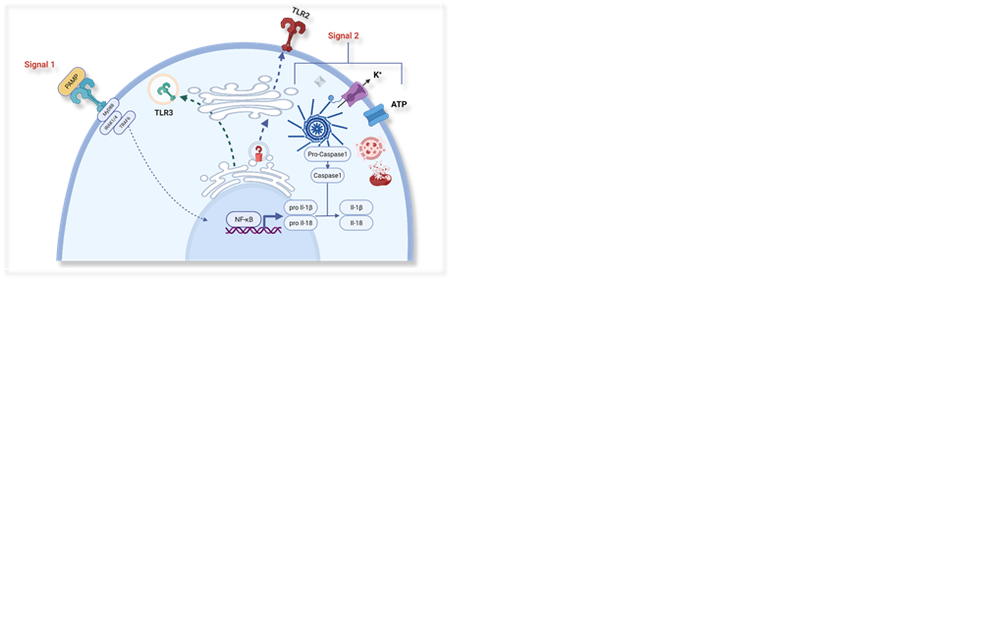
In our laboratory at the Department of Anaesthesiology and Intensive Care Medicine, we investigate the abnormalities in signal transduction responses caused by and causative for sepsis in both immune and parenchymal stromal cells. We use different approaches, e.g., in vitro model systems for organ damage or the analysis of genetic paediatric syndromes that influence the host immune and inflammatory response. In this practical course, you will analyse the biological consequences of rare pathological variants of a critical regulator of Toll receptor and inflammasome signalling discovered in rare cases of paediatric encephalopathy. We will use a combination of biochemical and flow cytometric approaches and work with genetically modified cell lines that mimic the cellular phenotypes of patients. These experiments will give you an insight into how the mechanisms of a host immune response can be studied in the laboratory using state-of-the-art technologies.